Methacholine Challenge Test
Diagnosing Asthma Through Methacholine Challenge Tests

The methacholine challenge test is used in several situations:
If the diagnosis of asthma is in question, eg, if the patient has symptoms that suggest asthma (either typical symptoms such as coughing, wheezing, and dyspnea or atypical symptoms) but normal results on regular spirometric testing and no response to a bronchodilator. Because the test has a high negative predictive value, it is more useful in ruling out asthma (if the result is negative) than in ruling it in (if the result is positive). A negative methacholine challenge test nearly rules out asthma; however, a positive test result needs to be interpreted cautiously if the patient is not experiencing symptoms.
In establishing a diagnosis of occupational asthma. For patients with remitting and relapsing symptoms suggestive of asthma associated with a particular work environment, a detailed history, physical examination, and methacholine challenge test can establish the diagnosis. Specific bronchial challenge testing with the suspected offending agent is possible, although this is more frequently used in research and in situations with significant legal or financial implications for the patient, such as workers' compensation cases.
Possibly, in managing asthma. In several clinical trials, outcomes were better when asthma management decisions were based on airway hyperresponsiveness combined with conventional factors (symptoms and lung function) than with management based on conventional factors alone. These findings suggest that asthma management based on serial measurement of airway hyperresponsiveness may be useful in optimizing outcomes of care; however, adjustment in treatment according to response to serial methacholine challenge tests is currently not recommended for routine management of asthma. In clinical research.
Obstruction Can be Improved or Provoked
Asthma is a chronic inflammatory disorder of the airways associated with characteristic clinical symptoms of wheezing, chest tightness, breathlessness, and cough. These symptoms may be associated with airflow limitation that is at least partially reversible, either spontaneously or with treatment.

Spirometry can confirm the diagnosis of asthma if lung function improves after a bronchodilator is given, as reflected by an increase in forced expiratory volume in 1 second (FEV1) of more than 12% and more than 0.2 L. Conversely, during bronchoprovocation testing, airflow obstruction is provoked by a stimulus known to elicit airway narrowing, such as inhaled methacholine. Bronchial hyperresponsiveness can reliably distinguish patients with asthma from those without asthma.

How the Test is Done
During the test, the patient inhales methacholine aerosols in increasing concentrations; various protocols can be used. Spirometry is performed before and after each dose, and the results are reported as a percent decrease in FEV1 from baseline for each step of the protocol.
A positive reaction is a 20% fall in FEV1, and the provocative concentration that causes a positive reaction (the PC20) is used to indicate the level of airway hyperresponsiveness. If the FEV1 does not fall by at least 20% with the highest concentration of methacholine, the test is interpreted as negative and the PC20 is reported as “more than 16 mg/mL” or “more than 25 mg/mL,” depending on the highest dose given. The maximum dose of methacholine varies among pulmonary function testing laboratories and asthma specialists; final doses of 16, 25, and 32 mg/mL are commonly used. Studies have defined a range of 8 to 16 mg/mL as an optimal cutoff point to separate patients with asthma from those without asthma.
The response to methacholine can also be expressed in terms of specific airway conductance; however, this is more complicated and requires body plethysmography.
Other stimuli that can be used as bronchoprovocation challenges to diagnose asthma include inhaled histamine, exposure to cold air, or eucapneic hyperventilation. Compared with these alternative stimuli, methacholine is the most feasible as it does not require extensive equipment and is better tolerated than histamine.
Potential Complications
Methacholine elicits airway narrowing in susceptible people and can cause severe bronchoconstriction, hyperinflation, or severe coughing. However, this procedure is generally well tolerated, and respiratory symptoms in patients who react to methacholine typically reverse promptly in response to bronchodilators.
Nevertheless, the test should be performed in a pulmonary function laboratory or doctor’s office with available personnel trained to treat acute bronchospasm and to use resuscitation equipment if needed. Informed consent should be obtained and recorded in the medical record after a detailed explanation of the risks and benefits of this procedure and alternatives to it.
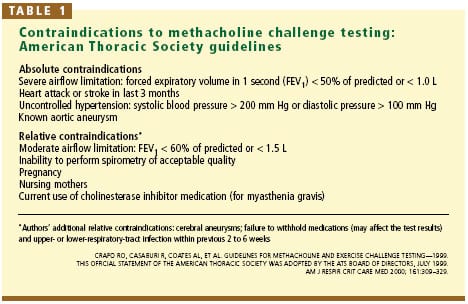
Contraindications
TABLE 1 summarizes the absolute and relative contraindications to this test.
Baseline obstruction. A ratio of FEV1 to forced vital capacity less than 70% on baseline spirometry defines airway obstruction, and methacholine challenge for diagnostic purposes would not be indicated.
Furthermore, patients with low baseline lung function, who may not be able to compensate for a further decline in lung function due to methacholine-induced bronchospasm, are at increased risk of a serious respiratory reaction. For this reason, an FEV1 less than 50% of predicted or less than 1.0 L is an absolute contraindication to methacholine challenge testing, and an FEV1 less than 60% of predicted or less than 1.5 L must be evaluated on an individual basis.
Myocardial infarction or stroke within the previous 3 months, uncontrolled hypertension, and aortic or cerebral aneurysm are absolute contraindications to this procedure, since induced bronchospasm may cause ventilation-perfusion mismatching resulting in arterial hypoxemia and compensatory changes in blood pressure, cardiac output, and heart rate. There is no increased risk of cardiac arrhythmia during methacholine challenge.
Pregnancy is a relative contraindication to methacholine challenge testing; methacholine is classified in pregnancy category C. Inability to perform spirometry correctly is also a relative contraindication, and therefore this test is not recommended for preschool-age children.
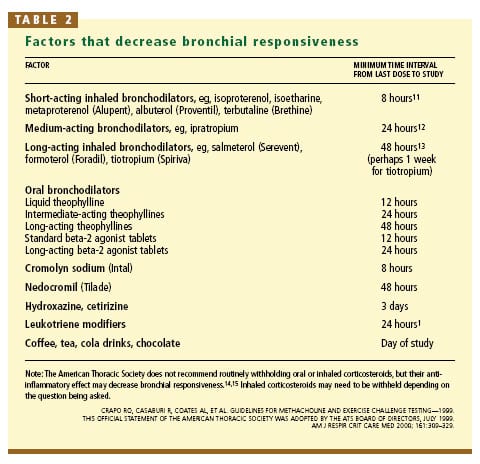
Some Drugs Should be Held
For this test to yield accurate results, the patient should not take any medications that would mask the response. The most common reason for canceling the test is lack of adequate patient preparation. Generally, the recommended periods for withholding medications are based on their duration of action (TABLE 2).
Other factors that can confound the results include smoking, respiratory infection, exercise, and consumption of caffeine (coffee, tea, chocolate, or cola drinks) on the day of the test. Airway responsiveness may worsen due to exposure to allergen or upper airway viral infections. Vigorous exercise could induce bronchoconstriction; therefore, performing other bronchial challenge procedures or exercise testing immediately before methacholine challenge may affect the results.
Bronchial hyperresponsiveness is seen in a variety of disorders other than asthma, such as smoking-induced chronic airflow limitation, congestive heart failure, sarcoidosis, cystic fibrosis, and bronchiectasis, as well as in siblings of asthmatics and in people with allergic rhinitis. In these situations, the methacholine test can be falsely positive, and one should interpret the results in the context of the clinical history.
Disclaimer:
Adapted from Medline plus, a service of the US National Library of Medicine and NIH